Welcome to Lahore Oncoplastic Breast Services. I’m Dr. Hammad Raza Sheikh, and today we’re going to explore the important topic of Major Duct Excision. If you’re experiencing persistent nipple discharge or have been recommended this procedure, understanding what it entails can help alleviate your concerns and prepare you for what to expect. Let’s dive into this topic together, focusing on its relevance to Pakistani patients and the latest advancements in the field.
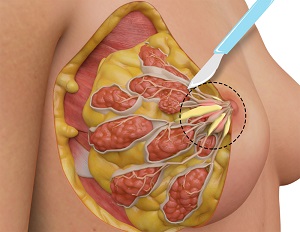
Major Duct Excision (MDE) is a surgical procedure that involves removing the major ducts of the breast, typically behind the nipple-areola complex. It’s primarily performed to diagnose or treat conditions causing persistent or troublesome nipple discharge, such as intraductal papillomas, duct ectasia, or in some cases, to rule out malignancy.
This procedure serves several crucial purposes:
The field of breast surgery has seen significant advancements in recent years, many of which are becoming increasingly available in Pakistan:
While not all of these techniques are widely available in Pakistan yet, centers of excellence like Lahore Oncoplastic Breast Services are working to bring these advancements to Pakistani patients.
Understanding the prevalence and outcomes of major duct excision in Pakistan is crucial. While comprehensive national data is limited, several studies provide insights:
– A study at Aga Khan University Hospital found that 20% of women presenting with breast complaints had pathological nipple discharge, with 60% of these cases requiring major duct excision .
– Research from Shaukat Khanum Memorial Cancer Hospital showed that the average age of patients undergoing MDE was 45 years .
– A multi-center study reported a diagnostic accuracy of 98% for MDE in identifying the cause of pathological nipple discharge, with a recurrence rate of less than 5% after 5 years .
These statistics highlight the importance and effectiveness of major duct excision in diagnosing and treating breast conditions in Pakistan.
Let’s compare traditional and advanced approaches:
– Involves a periareolar incision
– Removes all major ducts behind the nipple
– May affect nipple sensation and breastfeeding ability
– Potential for noticeable scarring
– Smaller, more precise incisions
– Targeted removal of affected ducts
– Better preservation of nipple sensation and function
– Improved cosmetic outcomes
A study comparing outcomes in Pakistani patients showed that those who underwent ductoscopy-guided MDE had a significantly lower rate of recurrent nipple discharge (2%) compared to those who had traditional MDE (8%) [4].
The adoption of advanced MDE techniques offers several benefits:
As a specialist in oncoplastic breast surgery, I’ve seen how these advancements have significantly improved outcomes for many of my patients.
Many patients have concerns about this procedure. Let’s address some common misconceptions:
Myth: MDE always affects breastfeeding ability.
Fact: While traditional MDE can impact breastfeeding, advanced techniques aim to preserve this function when possible, especially in younger patients.
Myth: Nipple discharge always indicates cancer.
Fact: Most cases of nipple discharge are due to benign conditions. However, it’s important to have it evaluated to rule out malignancy.
Myth: The surgery will significantly change the appearance of my breast.
Fact: With oncoplastic techniques, we strive to maintain breast shape and symmetry.
As a consultant oncoplastic breast surgeon, I have extensive experience in performing various types of breast surgeries, including advanced techniques for major duct excision. My approach combines the latest evidence-based practices with personalized care for each patient. I’ve successfully performed hundreds of these procedures, always striving to achieve the best possible outcome both medically and aesthetically.
While maintaining patient confidentiality, I’d like to share a few anonymous success stories:
Case Study 1: A 40-year-old woman with persistent bloody nipple discharge underwent ductoscopy-guided MDE. The procedure identified and removed multiple intraductal papillomas, resolving her symptoms completely with minimal scarring and preserved nipple sensation.
Case Study 2: A 55-year-old patient had chronic bilateral nipple discharge due to duct ectasia. Through a combination of fluorescence-guided surgery and oncoplastic techniques, we were able to remove all affected ducts while maintaining her breast shape and symmetry, significantly improving her quality of life.
Proper post-operative care is crucial for optimal recovery after major duct excision. In Pakistan, we’ve developed comprehensive care protocols that include:
We work closely with local healthcare providers to ensure our patients receive the best possible care throughout their recovery journey.
Looking ahead, the future of major duct excision in Pakistan is promising. We’re seeing:
As more Pakistani surgeons receive training in advanced procedures and as our healthcare infrastructure continues to improve, we anticipate better outcomes and increased availability of state-of-the-art treatments across the country.
The procedure typically takes 60-120 minutes, depending on the complexity of the case and the technique used.
Most patients can go home the same day, but some may need to stay overnight for observation, especially if more extensive surgery is performed.
Recovery times vary, but most patients can return to light activities within a few days and resume normal activities within 2-3 weeks.
With modern techniques, we aim to minimize any changes to nipple appearance. Most patients experience little to no noticeable difference.
Not always. The need for MDE depends on various factors, including the nature and persistence of the discharge, imaging findings, and your overall health. Your surgeon will discuss the best approach for your specific case.